Heart Failure With Preserved Ejection Fraction: An Update from the ACC 2023 Guidelines
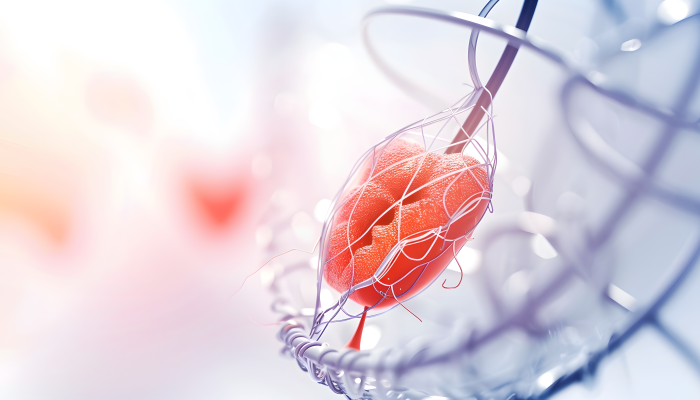
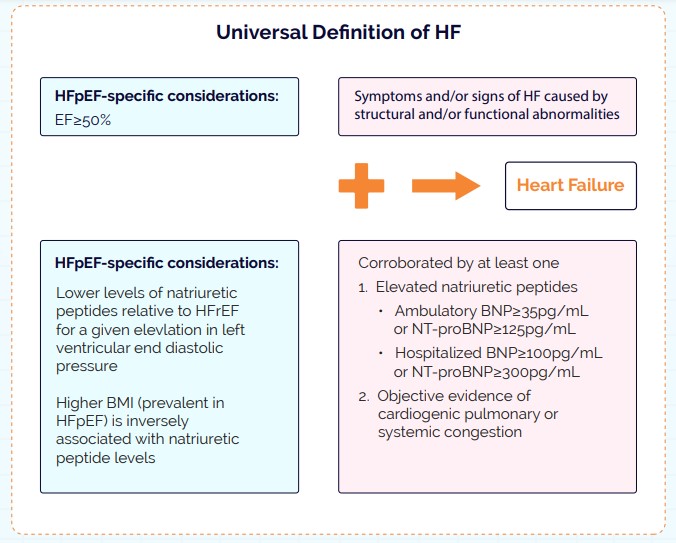
Heart Failure with preserved Ejection Fraction (HFpEF) is a form of heart failure characterized by the heart’s inability to relax and fill properly despite a normal or near-normal ejection fraction. It is often associated with diastolic dysfunction and is prevalent in elderly patients, particularly those with comorbidities such as hypertension, diabetes, and obesity. HFpEF is a complex, multifactorial syndrome that poses diagnostic and therapeutic challenges, given its diverse pathophysiology and the absence of specific, widely effective treatments.
HFpEF Diagnostic Scoring Systems
Utilizing clinical scoring systems can be beneficial in the diagnostic evaluation of suspected HFpEF. Both the H2FPEF and HFA-PEFF algorithms employ scoring methods to assess the likelihood that HFpEF is the underlying cause in patients presenting with dyspnea.
HFpEF Diagnostic Scoring System- H2 FPEF
| H2 | Heavy (BMI>30kg/m2) | 2 |
|---|---|---|
| On ≥2 antiHypertensives | 1 | |
| F | Atrial Fibrillation | 3 |
| P | Pulmonary Hypertension (PASP>35mm of Hg on Doppler Echocardiography) | 1 |
| E | Elder (age >60 years) | 1 |
| F | Filling pressure (E/e>9 on Doppler 1 Echocardiography) | 1 |
| ≥6 points: highly diagnostic of HFpEF |
HFA-PEFF Score
The HFA-PEFF score is a stepwise diagnostic tool for evaluating suspected
HFpEF: Pretest Assessment (P): Initial evaluation based on heart failure symptoms, risk factors, and standard echocardiography.
Echo and Natriuretic Peptide Score (E): Uses comprehensive echocardiography and natriuretic peptide levels to refine the diagnosis. Key parameters include functional, morphological, and biomarker criteria.
Functional Testing (F1): Recommended if uncertainty remains, involving diastolic stress tests or invasive hemodynamic measurements.
Final Etiology (F2): Further investigation through advanced imaging, biopsies, or genetic testing to confirm the diagnosis.
A score of 5 or more indicates a high likelihood of HFpEF, with major and minor criteria contributing to the score.
How to Manage HFpEF?
Management of HFpEF centers on three key areas:
- Risk Stratification and Comorbidity Management: Addressing hypertension, diabetes, obesity, atrial fibrillation, coronary artery disease, chronic kidney disease, and obstructive sleep apnea.
- Nonpharmacological Interventions: Emphasizing the importance of exercise, weight loss, and the use of wireless, implantable pulmonary artery monitors.
- Symptom Management and Disease-Modifying Therapies: Utilizing loop diuretics, SGLT2 inhibitors, mineralocorticoid receptor antagonists (MRAs), angiotensin receptor-neprilysin inhibitors (ARNIs), and angiotensin receptor blockers (ARBs)
Guideline-Directed Medical Therapy for HFpEF
Medical therapy for HFpEF inlcudes perindopril, irbesartan, beta-blockers, nitrates, digoxin, ivabradine, sildenafil, and serelaxin. Recent clinical trials have shown that guideline-directed medical therapy (GDMT) can benefit individuals with HFpEF, making the initiation of key agents crucial for improving symptoms, functional capacity, and reducing heart failure-related morbidity and mortality. GDMT is safe and effective in both acute and chronic-care settings.
Diuretics should be used carefully to alleviate congestion and improve symptoms. Beta-blockers may be prescribed for HFpEF patients with specific indications, such as recent myocardial infarction (up to three years), angina, or atrial fibrillation, but exercise tolerance must be monitored due to the risk of chronotropic incompetence
| Starting and Target Doses of Select GDMTs for HFpEF | ||
|---|---|---|
| Drug Class | Starting Dose | Target Dose |
| SGL T2is | ||
| Dapaglifozin | 10 mg daily | 10 mg daily |
| Empagliflozin | 10 mg daily | 10 mg daily |
| Aldosterone antagonists | ||
| Spironolactone | 25 mg daily | 50 mg daily |
| ARNIs | ||
| Sacubitril/valsartan | 24 mg/26 mg twice daily | 97 mg/103 mg twice daily |
| ARBs | ||
| Candesartan | 4 mg to 8 mg daily | 32 mg daily |
| ARB = angiotensin receptor blocker; ARNI = angiotensin receptor-neprilysin inhibitor; GDMT = guideline directed medical therapy; HFpEF = heart failure with preserved ejection fraction; SGLT2 = sodium-glucose cotransporter |
Treatment Algorithm for Guideline-Directed Medical Therapy in HFpEF
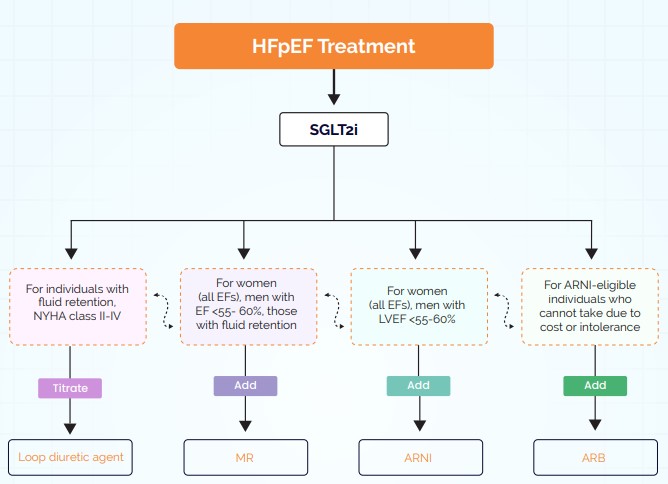
In the absence of contraindications, all patients with HFpEF should be treated with an SGLT2 inhibitor to reduce cardiovascular death and HF hospitalization, and to improve overall health status. SGLT2 inhibitors may be initiated for both ambulatory patients with HFpEF and those with acutely decompensated HF. For patients with an LVEF <55% to 60%, the use of MRA ARNI or ARB (if ARNI is not feasible) may be considered based on evidence strength and recent comparisons between ARNI and ARB. ARNIs and MRAs should be titrated to the maximum tolerated doses, considering symptoms, blood pressure, potassium levels, and creatinine, as recommended by the STRONG HF study.
How to Manage Co-Morbidities Associated with HFpEF?
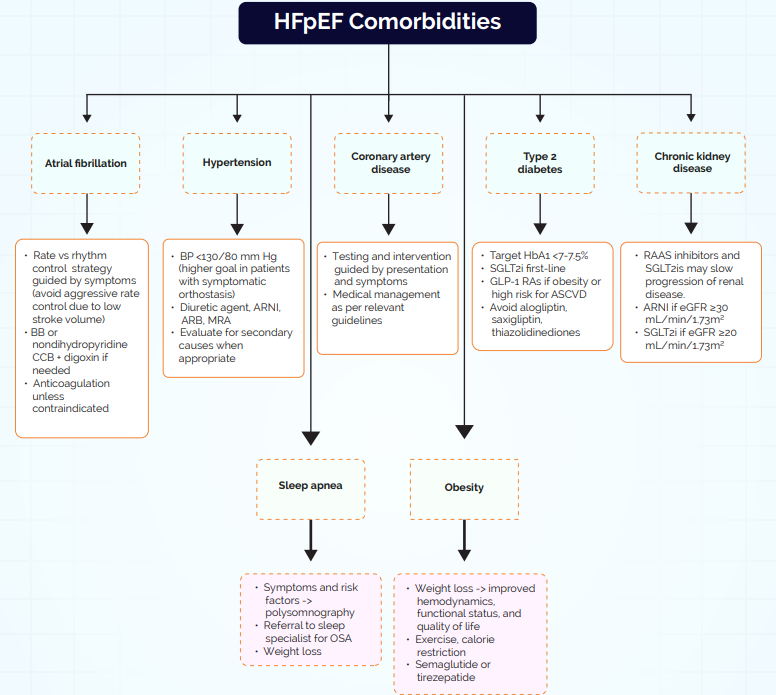
Despite confirming a diagnosis of HFpEF, several therapeutic challenges persist. Clinicians must address comorbidities affecting symptoms and prognosis, explore nonpharmacological strategies to alleviate symptoms, and implement guideline-directed medical therapy (GDMT) to enhance quality of life, reduce both HF and non-HF hospitalizations, and improve survival. Effective care demands a multidisciplinary approach. Given the diagnostic complexities and advancements in treatment, there is a crucial opportunity to redefine the management of HFpEF.