You have been diagnosed colorectal cancer. You always knew cancer to be dreadful and that it caused bleeding. You never noticed even a streak of blood in stool. You just felt a little unwell and had some alteration in stool frequency. It is hard to believe this can be cancer but a battery of investigations support the diagnosis. The next challenge is to treat it to the best extent possible. Your doctor has discussed with you what stage your cancer has and has explained the prognosis. Besides a medical challenge, you face an emotional challenge too. It is time you know more about it.
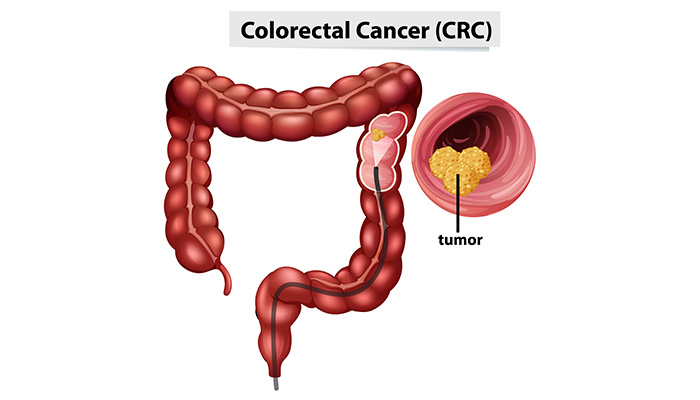
Understanding cancers of colon and rectum
Colon and rectum are the parts of the large intestine in our bellies. The large intestine is the main site of absorption of water from the food that we consume after the nutrients have been absorbed in the small intestines. Rectum is the terminal part of the large intestine where the fecal matter is stored. When it distends to a sufficient size, it gives us an urge to defecate and stools are then expelled through the anus. Cancer of the colon and rectum, also called the colorectal cancer may manifest as change in the bowel habits like diarrhea or constipation, passing blood in your stool, abdominal discomfort, weakness, unexplained weight loss is common. A total of 1,42,570 cases of cancer of colon and rectum have been reported in the US this year.
Stages of colorectal cancer
Staging of a cancer determines the location and quantum of cancer in the body. It is based upon the types of component cells in cancer. Staging describes the extent, severity, and spread of cancer and forms a guideline for treatment of cancer. Cancers can spread via blood stream to distant body parts, when it is called metastasis or may spread via lymphatic system to the lymph nodes. The lymphatic system is a specialized system of vessels that drain excess tissue fluids and have nodes interspersed that play a role in immunity and defense.
Stage 1: cancer means that the cancer has formed in the luminal inner most layer of the wall of the colon, called the mucosa and has extended to the space that lies underneath, called the submucosa.
Stage 2: cancer means that the cancer has spread to the third and the fourth layers of the colon wall, called the muscle layer and serosa, respectively. In late stage 2, it can even spread through the thickness of the serosa to involve the adjoining organs.
Stage 3: cancer essentially means that one or more of the lymph nodes draining the segment with cancer are involved. Lymph node involvement can be positive irrespective of the spread of cancer at the site to the mucosa, muscle layer or serosa.
Stage 4: cancer implies that metastasis are positive and the cancer has spread to distant organs like the liver, lung, lining of the abdominal wall, and others.
Treatment
Treatment of colorectal cancer is guided by the stage of the cancer, the health of the patient, and by the fact that the cancer is the first or a recurrent one. The options include treatment with medicines called chemotherapy or treatment by using special radiations to kill the cancer cells, called radiotherapy. Surgical removal of cancer may eventually be required. Biological therapy that comprises monoclonal antibodies, special proteins that target and kill the cancer cells, is also used. These antibodies are also produced in our bodies as defenses against cancerous cells or other harmful invaders. One or more of the treatment options can be used in combination of sequentially.
Chemotherapy implies use of drugs to kill the aberrant cancer cells. The drugs may be given by mouth or as an injection. Depending upon the stage of cancer, chemotherapy can be used alone or may be given with other treatment options. Generally, chemotherapy is used when cancer has spread beyond the wall of intestine or to lymph nodes. Another type of drugs, called monoclonal antibodies, may be used in some advanced cases. These specifically target the cancer cells and bind to them to arrest their division. Side effects occur when treatment targeted to cancer cells also affects the normal cells in the body. There can be fatigue or loss of appetite. Chemotherapy can cause diarrhea, vomiting, hair loss, sores in mouth, easy bruising, rash and swelling in hands and feet.
High energy rays can be used to kill the cancer cells. The source of radiation may be outside the body (external radiation) or radioactive materials may be placed in the tumor area (brachytherapy or internal or implant radiation). Radiotherapy may be used before surgery to shrink the tumor size and make it resectable, during surgery to hit the small cancerous foci, or after surgery to kill the residual tumor. Radiotherapy is best used for the cancer that has gone beyond the intestinal wall to the adjacent organs. Radiotherapy may turn the exposed skin sore and red. It can also cause vomiting or a sensation of one, diarrhea, blood in stools, and urinary and sexual problems. The effects may reverse upon discontinuation of treatment.
Clinical research programs
Clinical research programs are investigations for novel treatments of a disease conducted in centers authorized to do them. Healthy volunteers and patients can chose to participate in a clinical research. Such research is conducted as per protocol and has specifications about who can or cannot participate in the program.
After treatment
If you have undergone a treatment or a surgical removal for colon cancer, you may need to undergo periodic tests to detect the blood counts or other organs functions like the liver and kidney function tests. Additionally, you may be advised to undergo testing for carcinoembryonic antigen (CEA) (normal levels: 2.5 to 3 ng/mL) to detect recurrences. CEA testing may be done bimonthly or less frequently depending upon the stage of cancer.
Prognosis
Prognosis, which implies the likelihood of recovery, is determined by the stage of cancer, the number of recurrent episodes, resectability of a focus of cancer, CEA levels, and the overall health of the patient. The cancers that have spread to distant sites have the gravest prognosis.
Living with colorectal cancer
Timely detection and appropriate treatment can improve life in colorectal cancer. However challenging the treatment may be, if you are prepared to meet it, you can make it more effective. Discuss more with your doctor and learn about the stage of your cancer and what treatment may be required. After you have been treated, religiously adhere to the follow up plan. You may need to undergo regular physical examinations, blood tests, scans and examination of the intestines with fiber optic flexible tubing inserted way up the anal opening. If you have undergone a surgical resection, you will need to know how to do without the segment of your intestine that you have lost. You need to plan for healthy survivorship. You may seek help of family and friends and even join a support group.