Pulmonary embolism (PE) is the third leading cause of cardiovascular death with high mortality rates. Systemic thrombolysis is the preferred treatment but increases bleeding risk, especially in older patients. While effective for high-risk, unstable patients, its benefits are uncertain in intermediate-risk patients without hemodynamic instability
What are the Challenges with Systemic Thrombolysis?
Meta-analysis shows no significant reduction in mortality for intermediate-risk PE patients using full-dose thrombolytics and highlights associated bleeding risks. Many high-risk PE patients have contraindications to systemic thrombolysis, necessitating alternative treatments.
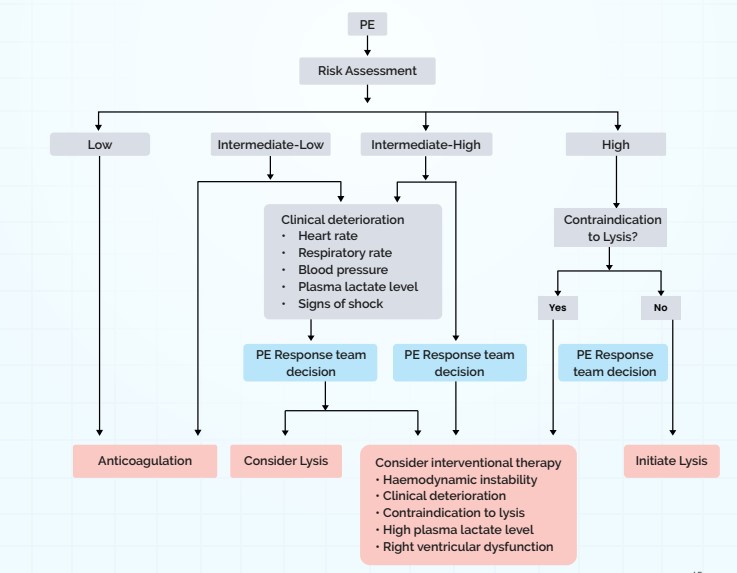
Algorithm for PE management (Chart)
What are the Interventional Therapies Available for PE?
- Catheter-Directed Thrombolysis (CDT): In CDT, thrombolytic medication is administered directly into the pulmonary arteries via catheters. This approach minimizes the overall dosage of the thrombolytic agent and may decrease the risk of bleeding complications.
- Ultrasound-Assisted CDT (USCDT): In USCDT, high-frequency ultrasound is used alongside thrombolytic drugs to break apart fibrin strands. This process increases the thrombus surface area, enhancing the effectiveness of the thrombolytic treatment.
- Pharmacomechanical CDT: In pharmacomechanical CDT, thrombi are mechanically fragmented and simultaneously dissolved using thrombolytic agents. The catheters are equipped with mesh baskets and side ports for delivering thrombolytics. As the thrombus in the pulmonary artery is dissolved, the basket expands to ensure continuous contact with the remaining clot.
- Aspiration Thrombectomy: In aspiration thrombectomy, thrombi in the pulmonary artery are removed using suction via catheters connected to a negative pressure pump or a syringe. Access to the pulmonary artery is achieved percutaneously through femoral or jugular veins. Aspiration is performed once the catheter is positioned near the thrombus. In large-bore aspiration thrombectomy, 16–24 F catheters are used, which are also equipped with a syringe. Special discs can be introduced through these large-bore catheters to fragment and capture thrombi for subsequent removal

What are the current guidelines related to Interventional Therapies in PE?
- As per the 2019 ESC Guidelines, interventional therapies are recommended for:
– Intermediate–high-risk PE with worsening symptoms despite anticoagulation.
– High-risk PE if thrombolysis fails or is contraindicated (Class IIa, Level C evidence). - AHA notes potential for interventional therapies in high-risk PE with lysis contraindications, but data on outcomes is limited.
- 2021 CHEST Guidelines suggest interventional therapies for high-risk PE with shock, high bleeding risk, or failed thrombolysis.
- 2022 ESC Consensus highlights a potential role for these therapies at specialized centers, despite limited data.